Preventive Medicine Resident
School of Medicine and Public Health
Look at this picture:
DF-12054 – Kate Mara as Sue Storm and Michael B. Jordan as Johnny Storm face off against an incredibly powerful enemy. Photo Credit: Ben Rothstein - From: http://www.nerdreport.com/2015/08/06/fantastic-four-movie-review-paved-with-good-intentions/
What is the relationship between those two characters??
Are they friends? Are they teammates? Are they family? Are they a couple?
If you know the movie - or the original source - you know that they are siblings. For some reason the only explanation for different skin color was that one of them was adopted, because siblings can’t be of different skin color, right?
Now think about this:
A father and his son are in a car accident. The father dies at the scene and the son is rushed to the hospital. At the hospital the surgeon looks at the boy and says "I can't operate on this boy, he is my son." How can this be?
If you thought "This is an identification issue, maybe an Uncle? Step-father? God-Father?" before you said "The surgeon is the mother" then you might be biased about how a physician looks like. (You can find many examples of situations where these biases were used: #IlookLikeASurgeon #WhatADoctorLooksLike)
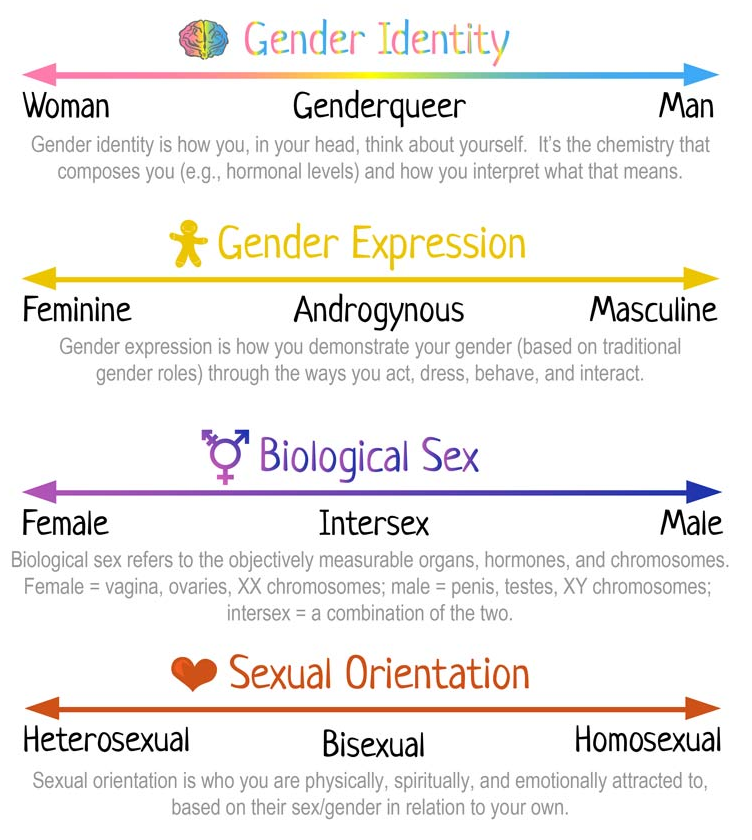
The point is, that we are all biased (it is OK, it happens, don’t feel guilty about it) and you can take a test (The Implicit Association Test (IAT)) to identify your biases (Race, gender, sexual orientation, weight, religion, and many more). You can read some research regarding this test here.
Bias occurs in everyone (Physicians too, e.g. here, and here). Although we are not sure WHY it happens, some experts believe it is related to our tendency to categorize, and that some associations (e.g. latino=lazy, black=bad, women=nurturing, women=homemaker) might be a result of our experiences, and media exposures (e.g. here, here, and here). What we know is that bias can affect behavior, so it is important to recognize them and make sure we don’t act based on those biases.
I am biased. What should I do now?
From the Project Implicit website:
“It is well-established that implicit preferences can affect behavior. But, there is not yet enough research to say for sure that implicit biases can be reduced, let alone eliminated. Therefore, we encourage people not to focus on strategies for reducing bias, but to focus instead on strategies that deny implicit biases the chance to operate. One such strategy is ensuring that implicit biases don’t leak out in the first place. To do that, you can “blind” yourself from learning a person’s gender, race, etc. when you’re making a decision about them (e.g., having their name removed from the top of a resume). If you only evaluate a person on the things that matter for a decision, then you can’t be swayed by demographic factors. Another strategy is to try to compensate for your implicit preferences. For example, if you have an implicit preference for young people you can try to be friendlier toward elderly people. Although it has not been well-studied, based on what we know about how biases form we also recommend that people consider what gets into their minds in the first place. This might mean avoiding television programs and movies that portray women and minority group members in negative or stereotypical ways”.
My personal take: Keep an open mind, what could be logical/normal for you might not be so normal for others and vice versa, avoid assumptions until you know the full story, and don’t act on your biases!
This blog was inspired by my attendance to a meeting titled Unlearning Racism hosted by YWCA Southeast Wisconsin, which was part of the monthly meetings of the Wisconsin Population Health Service Fellowship. At this meeting, we learned about the history of systemic racism and how biases affect behavior and lead to disparities in health and health care. If you would like to read about these topics check the following resources:
Unpacking the Invisible Knapsack by Peggy McIntosh
Toward a Cultural Consciousness of Self in Relationship: From “Us and Them” to “We” by William Ventres and Cynthia Haq